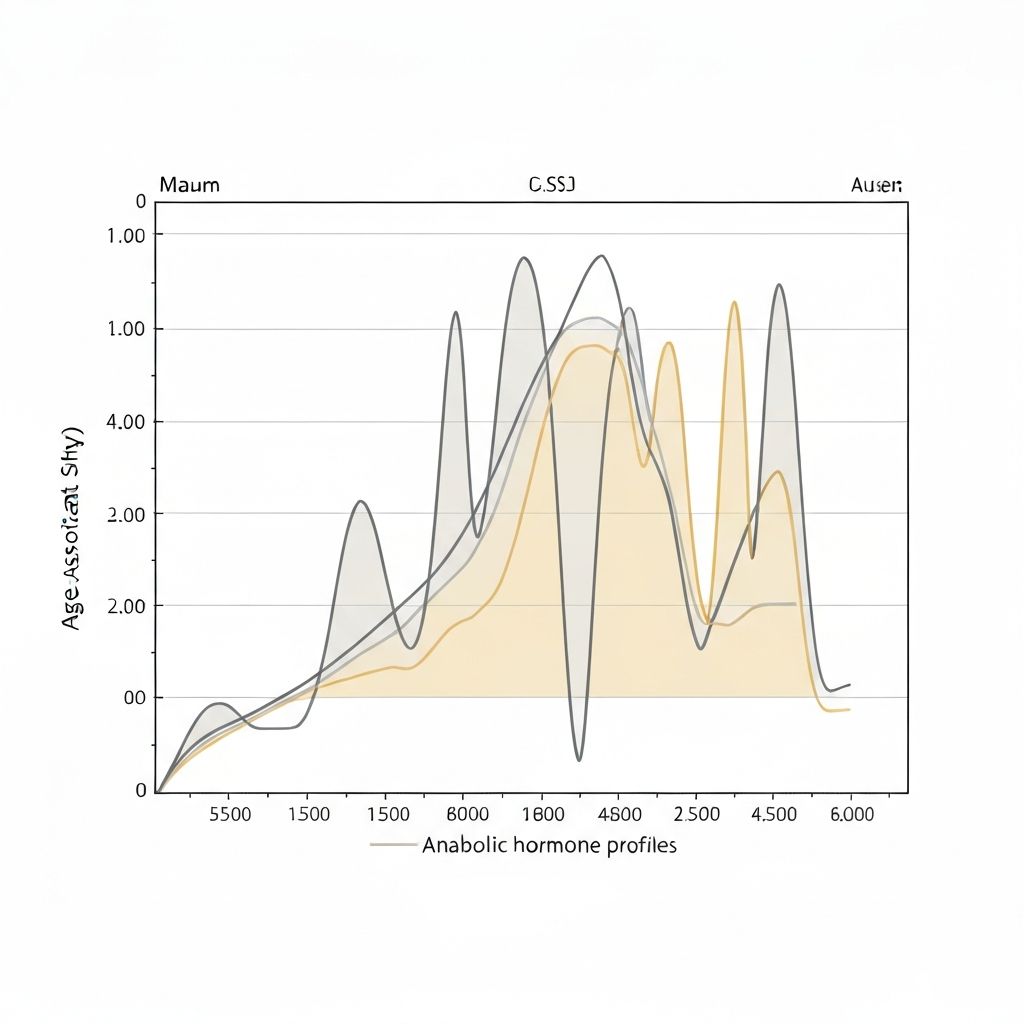
Age-Associated Shifts in Anabolic Hormone Profiles
Growth hormone, testosterone, and IGF-1 changes across the lifespan
Overview of Anabolic Hormones
Anabolic hormones promote protein synthesis, lean mass development, and energy production. Key hormones in this category include growth hormone (GH), testosterone, and insulin-like growth factor 1 (IGF-1). These hormones work synergistically to support muscle protein synthesis, bone formation, metabolic rate, and overall metabolic health.
Growth Hormone Patterns Across the Lifespan
Growth hormone (somatotropin) is secreted by the anterior pituitary gland in response to growth hormone-releasing hormone (GHRH) from the hypothalamus. It is released in pulsatile patterns, particularly during sleep and after resistance exercise.
Growth hormone levels follow a consistent pattern across the lifespan:
- Peak Levels: Highest during adolescence and early adulthood
- Decline Rate: Decreases approximately 10-15% per decade after age 30
- Age 40: Growth hormone levels are noticeably lower than at age 20
- Age 60: Growth hormone secretion may decline to 30-50% of young adult levels
This gradual decline is considered a normal aspect of aging physiology rather than a pathological state. The decline reflects changes in hypothalamic function, growth hormone-binding proteins, and altered responsiveness to stimuli.
Functions affected by declining growth hormone include protein synthesis promotion, lipolysis stimulation (fat breakdown), and metabolic rate regulation. The gradual decline contributes to metabolic changes observed during midlife.
Testosterone Changes with Age
Testosterone is an anabolic steroid hormone produced primarily in the testes (in men) and adrenal glands and ovaries (in women). It is essential for muscle protein synthesis and lean mass maintenance in both sexes, though levels differ substantially between men and women.
- In Men: Testosterone levels peak during late teenage years and early adulthood. After age 30, levels decline approximately 1% per year on average, though individual variation is substantial. By age 70, average testosterone levels may be 20-40% lower than at age 20.
- In Women: Testosterone levels are lower than in men throughout life. Levels remain relatively stable during reproductive years but decline during perimenopause and postmenopause. Ovarian production declines, though adrenal production continues.
Declining testosterone contributes to reduced muscle protein synthesis capacity, potentially accelerating sarcopenia. However, testosterone levels remain adequate for muscle maintenance in most healthy adults, and other factors (physical activity, protein intake) play important roles in preserving lean mass.
Insulin-Like Growth Factor 1 (IGF-1)
IGF-1 is a peptide hormone produced primarily in the liver (in response to growth hormone stimulation) and in peripheral tissues including muscle. It works synergistically with growth hormone to promote protein synthesis, cell growth, and metabolic effects.
IGF-1 patterns across the lifespan:
- Peak Levels: Highest during adolescence (concurrent with growth hormone surge)
- Young Adulthood: Levels decrease gradually from peak
- After Age 40: IGF-1 levels continue to decline slowly, roughly 14% per decade in some studies
- Age-Related Changes: Declining growth hormone reduces IGF-1 production; changing IGF-1 binding protein concentrations affect free (active) IGF-1 levels
IGF-1 supports muscle protein synthesis, carbohydrate metabolism, and bone formation. Declining IGF-1 contributes to reduced capacity for muscle protein synthesis and increased risk of sarcopenia.
Hormonal Patterns and Metabolic Implications
The coordinated decline in growth hormone, testosterone, and IGF-1 creates a physiological context in which:
- Muscle protein synthesis capacity declines, making lean mass preservation more metabolically challenging
- Metabolic rate gradually decreases due to lower anabolic signalling
- Fat distribution patterns shift toward increased visceral adiposity
- Glucose metabolism and insulin sensitivity may be affected
- Bone density formation may decline
These changes are not "failures" of the endocrine system but rather normal physiological aging patterns documented consistently across human populations.
Stimulation of Hormone Production
Certain lifestyle factors influence anabolic hormone production and responsiveness:
- Resistance Training: Stimulates growth hormone release and increases growth hormone receptor expression in muscle tissue
- Sleep Quality: Growth hormone is released primarily during deep sleep; poor sleep reduces growth hormone secretion
- Stress Management: Chronic stress elevates cortisol, which may suppress anabolic hormones
- Adequate Nutrition: Malnutrition reduces growth hormone and IGF-1 production
- Physical Activity: Regular activity supports hormone production and receptor function
While these factors can support hormone function, they do not reverse age-related hormonal decline. The changes reflect normal physiological aging rather than hormone deficiency requiring pharmaceutical intervention.
Individual Variation in Hormone Profiles
Substantial individual variability exists in baseline hormone levels and the rate of age-related decline. Genetics, health status, physical fitness, body composition, and stress levels all influence hormone concentrations. Some individuals maintain relatively higher hormone levels into midlife and beyond, while others experience more pronounced decline.
Educational Context
This article provides educational explanation of age-associated hormone changes. It does not constitute medical advice or endocrine assessment. Individual hormone assessment and interpretation require professional medical evaluation and should not be self-diagnosed or self-managed without professional guidance.